Degenerative diseases are on the rise, making it vital to understand the degeneration process for anyone concerned about health, longevity, and disease prevention in 2025. With new research uncovering hidden risks and early warning signs, staying informed has never been more crucial.
This guide will demystify the degeneration process, offering a clear overview of what it means, its causes, stages, prevention strategies, and the latest treatment advances. By reading, you’ll gain actionable insights to recognize, manage, and even slow degeneration in various tissues and systems—empowering you to take proactive steps toward long-term well-being.
Understanding the Degeneration Process
Understanding the degeneration process is key to making informed decisions about your health. Degenerative changes can occur in many tissues and systems, but recognizing their scope and impact is the first step toward prevention and management.
Definition and Scope of Degeneration
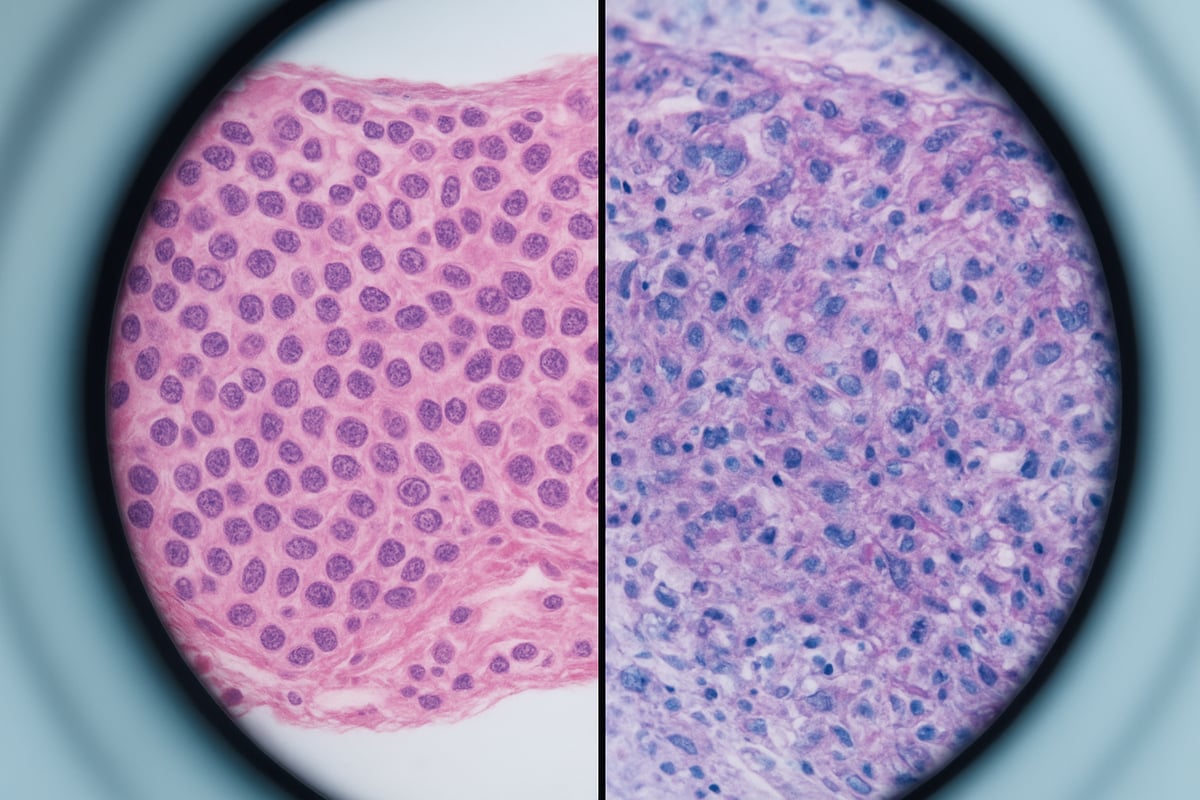
The degeneration process involves the gradual deterioration of cells, tissues, or organs, leading to impaired function. It is important to distinguish between normal aging, which all bodies experience, and pathological degeneration, which goes beyond typical wear and tear.
Degeneration can manifest at various levels:
- Cellular degeneration: Loss of cell structure or function.
- Tissue degeneration: Breakdown of connective tissues, such as cartilage.
- Organ degeneration: Decline in heart, brain, or eye function.
- Systemic degeneration: Widespread effects across multiple organ systems.
Common examples include osteoarthritis, neurodegeneration (like Alzheimer’s), retinal degeneration, and muscular atrophy. Globally, degenerative diseases are rising, affecting millions and significantly lowering quality of life. Early understanding of the degeneration process allows for timely intervention and improved outcomes.
Biological Mechanisms Behind Degeneration
At the heart of the degeneration process are several interconnected biological mechanisms. One key factor is cellular senescence, where aging cells lose their ability to divide and function. Apoptosis, or programmed cell death, also contributes to tissue decline.
Oxidative stress, caused by free radicals, damages proteins, DNA, and cell membranes, accelerating tissue breakdown. Chronic inflammation acts as a silent driver, promoting ongoing damage in the background. Mitochondrial dysfunction leads to energy deficits, impairing cell survival.
Genetic predispositions and epigenetic changes set the stage for how quickly degeneration unfolds. For example, in Alzheimer’s disease, abnormal protein deposits (amyloid plaques) disrupt brain cell communication. According to the WHO, over 50 million people worldwide are affected by neurodegenerative conditions, reflecting the immense reach of these biological processes.
Understanding the degeneration process at this level helps researchers develop targeted therapies and preventive strategies. As science advances, we are learning how these molecular changes translate into the symptoms and disabilities seen in degenerative diseases.
Common Types of Degenerative Conditions
The degeneration process can affect nearly every system in the body, but some conditions are especially prevalent. Musculoskeletal degeneration, including osteoarthritis and osteoporosis, leads to joint pain and fractures. Neurological conditions like Parkinson’s disease, Alzheimer’s, and ALS cause movement and memory problems.
Ocular degeneration, such as macular degeneration and glaucoma, threatens vision for millions. Cardiovascular issues like heart valve degeneration and atherosclerosis increase the risk of heart attacks and strokes.
| Type | Example Conditions | Key Symptoms |
|---|---|---|
| Musculoskeletal | Osteoarthritis, Osteoporosis | Joint pain, fractures |
| Neurological | Parkinson’s, Alzheimer’s, ALS | Memory, movement loss |
| Ocular | Macular degeneration, Glaucoma | Vision loss |
| Cardiovascular | Valve degeneration, Atherosclerosis | Fatigue, chest pain |
Osteoarthritis alone affects 32.5 million adults in the US, according to the CDC. Each type of degeneration requires a tailored approach for prevention and treatment. For a deeper look at how the degeneration process impacts eye health, see this Degenerative Disease in Eyes Overview.
The Difference Between Acute and Chronic Degeneration
Not all degeneration progresses in the same way. Acute degeneration occurs suddenly, often after injury or a single damaging event, and may be reversible with prompt care. Chronic degeneration, by contrast, develops slowly over time, frequently going unnoticed until significant function is lost.
For example, acute cartilage injury can cause immediate joint pain, while chronic osteoarthritis gradually wears away cartilage, leading to stiffness and long-term discomfort. Treatment strategies differ based on whether the degeneration process is acute or chronic, with chronic forms often requiring ongoing management and rehabilitation.
Chronic degeneration is particularly challenging because symptoms may be subtle until advanced stages. This underlines the importance of early detection and intervention.
Societal and Economic Impact
The degeneration process does not just affect individuals; it has widespread implications for society. Healthcare systems face rising costs, with degenerative diseases being a leading cause of disability worldwide.
Productivity loss and the burden on caregivers are significant. For example, dementia care costs now exceed $1 trillion globally, according to the Alzheimer’s Association. The growing prevalence of degenerative conditions highlights the urgent need for improved prevention and treatment strategies.
Stages of the Degeneration Process
Understanding the stages of the degeneration process is essential for timely intervention and improved outcomes. By breaking down each phase, you can recognize patterns, act early, and potentially slow or manage disease progression.

Early Stage: Subtle Signs and Cellular Changes
The degeneration process begins at the molecular level, often before symptoms appear. Early changes include DNA damage, protein misfolding, and diminished cellular repair. These alterations may cause mild discomfort, low-grade fatigue, or subtle vision changes that are easy to overlook.
Regular screening and the use of biomarkers are crucial for detecting these early events. For example, early macular degeneration can be identified with advanced retinal imaging. New technologies, such as the ALS ‘disease-on-a-chip’ model developed, help researchers study the earliest phases of the degeneration process, offering hope for earlier diagnosis and intervention.
Progressive Stage: Structural and Functional Decline
As the degeneration process advances, tissues begin to break down, resulting in noticeable symptoms and functional impairments. This stage is marked by joint stiffness, memory lapses, or vision loss, depending on the specific condition.
Diagnostic tools like MRI scans can reveal cartilage loss in osteoarthritis or changes in brain structure in neurodegenerative diseases. Laboratory findings may show increased inflammatory markers or metabolic imbalances. Recognizing the progression at this stage allows for targeted therapies and lifestyle adjustments that can help slow further decline.
Advanced Stage: Irreversible Damage and Complications
In the advanced stage of the degeneration process, tissue or organ function may be permanently lost. Complications such as severe disability, dependence on others, and secondary illnesses become common.
Examples include end-stage heart failure, total vision loss from retinal degeneration, or profound cognitive decline in late-stage Alzheimer’s disease. Prognosis at this stage focuses on managing symptoms and maintaining quality of life. While some damage cannot be reversed, supportive care and rehabilitation are vital for preserving independence and dignity.
Factors Influencing Rate of Progression
The speed of the degeneration process varies widely between individuals. Age and genetics play significant roles, but lifestyle factors such as physical activity, diet, and management of chronic conditions are equally important.
Chronic inflammation, metabolic health, and environmental exposures like toxins or pollutants can accelerate tissue breakdown. Modifiable risk factors, including regular exercise and a balanced diet, can slow the progression. Understanding these influences empowers patients and clinicians to tailor prevention and intervention strategies.
Case Studies: Real-World Progression Paths
Comparing real-world cases highlights how the degeneration process can unfold differently. For instance, two patients with osteoarthritis may experience vastly different outcomes based on their activity levels and nutrition.
Longitudinal studies show that individuals who engage in regular exercise and maintain a healthy diet often have slower disease progression. Early intervention, personalized care plans, and consistent monitoring all contribute to better long-term results. These cases underscore the importance of proactive management in altering the course of degeneration.
Major Risk Factors and Causes of Degeneration
Understanding the major risk factors behind the degeneration process is essential for prevention and management. By recognizing these causes, individuals and healthcare professionals can develop more effective strategies to slow or even halt the progression of various degenerative conditions.

Genetic and Hereditary Influences
Genetics play a central role in the degeneration process. Family history and inherited gene mutations can increase vulnerability to specific degenerative diseases. For instance, mutations in the BRCA genes are linked to certain cancers, while the APOE4 gene increases Alzheimer's disease risk.
Studies reveal that up to 60% of macular degeneration cases are tied to genetic factors, highlighting the profound impact of heredity. Genetic screening enables earlier identification of at-risk individuals, allowing for tailored prevention plans.
Understanding your genetic makeup is a crucial step towards controlling the degeneration process. Early interventions, guided by genetic counseling, can make a significant difference in long-term outcomes.
Lifestyle and Environmental Contributors
Lifestyle choices and environmental exposures are powerful drivers of the degeneration process. Factors such as smoking, unhealthy diets, and physical inactivity can accelerate tissue breakdown and cellular aging.
Exposure to environmental toxins, including heavy metals and pesticides, further compounds risk. Urban living often increases contact with air pollution, which has been linked to higher rates of degenerative diseases.
For example, smokers are twice as likely to develop macular degeneration compared to non-smokers. Adopting healthier habits, such as regular exercise and a nutrient-rich diet, can reduce the likelihood of triggering the degeneration process.
Chronic Diseases and Comorbidities
Chronic health conditions have a direct impact on the degeneration process. Diseases like diabetes, hypertension, and autoimmune disorders can accelerate tissue degeneration through ongoing inflammation and metabolic disruption.
A well-known example is diabetic retinopathy, where prolonged high blood sugar leads to vascular degeneration in the eyes. The presence of multiple chronic diseases can further amplify the degeneration process, making management more complex.
Effectively controlling underlying health issues is vital. Proactive disease management not only enhances quality of life but also slows the degeneration process across various body systems.
Aging and Biological Wear
Aging is a natural contributor to the degeneration process, but the rate and severity can vary widely. Over time, telomeres shorten and cellular repair mechanisms become less efficient, leading to increased vulnerability.
However, not all degeneration is inevitable. Statistics show that 80% of people over 65 have at least one degenerative condition, yet lifestyle interventions can still make a meaningful difference. Distinguishing between normal aging and accelerated degeneration helps guide appropriate interventions.
By focusing on healthy aging strategies, individuals can manage the degeneration process and preserve function for longer periods.
Emerging Risk Factors in 2025
In 2025, new research has identified additional risk factors influencing the degeneration process. The human microbiome, chronic psychological stress, and increased digital device usage are now recognized as contributors to tissue decline.
Social determinants, such as socioeconomic status and access to healthcare, also shape individual risk profiles. For instance, blue light exposure from screens is linked to retinal health challenges.
Staying informed about evolving science is key. For ongoing updates and in-depth discussions on these topics, visit the Latest Blog Articles on Degeneration.
Early Detection and Warning Signs
Early detection is critical in the degeneration process, often determining whether interventions can slow or even reverse decline. Many degenerative conditions develop silently, making it vital to recognize early warning signs before significant damage occurs. In 2025, as the global burden of degenerative diseases rises, understanding these early signals empowers individuals and healthcare providers to act swiftly and effectively.
Recognizing Subtle Physical and Cognitive Changes
The degeneration process often begins with minor, easily overlooked changes. Early symptoms may include mild joint pain, occasional stiffness, slight vision disturbances, or brief memory lapses. These subtle shifts can be mistaken for normal aging, but they are sometimes the first signs of underlying degeneration.
Individuals should pay attention to persistent discomfort, changes in balance, or gradual decline in sensory abilities. Routine self-monitoring and regular health check-ups are crucial. For example, early glaucoma symptoms, such as peripheral vision loss, are often missed until advanced stages, highlighting the importance of vigilance in the degeneration process.
Diagnostic Tools and Screening Methods
Advances in medical technology have transformed early detection of the degeneration process. Imaging techniques like MRI, CT scans, and retinal imaging can reveal structural changes before symptoms become severe. Blood tests for inflammatory markers and genetic panels provide further insight, while functional assessments evaluate mobility, cognition, and vision.
Evidence shows that early detection improves outcomes by up to 40 percent, according to a 2023 Lancet report. As WHO warns of slowing global health gains, prioritizing regular screening is more important than ever in combating the rising prevalence of degenerative diseases. Early diagnosis allows for prompt intervention, potentially altering the trajectory of the degeneration process.
The Role of Biomarkers and Predictive Analytics
Biomarkers have become essential tools in identifying the onset of the degeneration process. Blood, saliva, and genetic biomarkers offer early clues about disease risk and progression. AI-driven predictive models now analyze these data points to forecast an individual's likelihood of developing certain degenerative conditions.
For example, blood tests can predict Alzheimer’s risk years before symptoms appear. This personalized approach enables tailored prevention strategies and more effective monitoring. As predictive analytics evolve, the degeneration process can be mapped out with increasing accuracy, allowing for earlier and more targeted interventions.
Importance of Family and Medical History
A thorough understanding of family and medical history is a powerful asset in the early detection of the degeneration process. Genetic counseling and detailed health records help identify individuals at higher risk for certain degenerative diseases. Knowing if relatives have conditions like macular degeneration or Alzheimer’s can prompt earlier screening and preventive care.
For families with hereditary conditions, early intervention can significantly delay or reduce disease progression. Discussing family health openly and maintaining updated records supports clinicians in identifying patterns and taking proactive steps against the degeneration process.
Barriers to Early Detection and How to Overcome Them
Despite advancements, several barriers hinder early detection of the degeneration process. Lack of awareness, limited access to screening, and fear of diagnosis often delay timely intervention. Stigma surrounding cognitive or physical decline can also prevent individuals from seeking help.
Solutions include public education campaigns, affordable and accessible screening programs, and community outreach. Empowering individuals with knowledge and resources encourages proactive health management. Overcoming these barriers not only saves lives but also reduces the long-term burden of the degeneration process on families and society.
Prevention and Lifestyle Strategies for Slowing Degeneration
Taking proactive steps to slow the degeneration process can make a significant difference in your quality of life and long-term health. By focusing on nutrition, exercise, stress management, environmental factors, regular check-ups, and social engagement, you can address multiple risk factors and support healthy aging.
Nutrition and Dietary Approaches
What you eat plays a crucial role in the degeneration process. Diets rich in antioxidants, such as fruits, vegetables, and omega-3 fatty acids, help combat cellular damage. The Mediterranean diet, for instance, has been shown to reduce the risk of neurodegeneration by 30 percent according to recent research.
Key dietary strategies include:
- Incorporating colorful produce like berries, spinach, and carrots.
- Consuming healthy fats from sources such as olive oil and fatty fish.
- Supplementing with nutrients like vitamin D, lutein, and zinc if advised by your healthcare provider.
A well-balanced diet not only supports the body’s repair mechanisms but can also help prevent conditions like age-related macular degeneration, illustrating the importance of food choices in the degeneration process.
Exercise and Physical Activity
Regular physical activity is one of the most effective ways to slow the degeneration process. Both aerobic and resistance training have proven benefits for maintaining joint, muscle, and brain health.
Recommended approaches:
- 150 minutes of moderate exercise per week, including walking, cycling, or swimming.
- Strength training two or more days a week to preserve muscle mass.
- Gentle practices such as tai chi, which enhance balance and joint flexibility.
Studies show that staying active can slow cartilage loss in osteoarthritis and support healthy aging throughout the degeneration process.
Managing Chronic Stress and Sleep
Chronic stress and poor sleep can accelerate the degeneration process by raising cortisol levels and interfering with cellular repair. It is important to manage stress for both mental and physical health.
Effective techniques include:
- Mindfulness meditation and deep breathing exercises.
- Cognitive behavioral therapy to manage negative thought patterns.
- Establishing a consistent sleep routine to enhance restorative rest.
Data indicates that people with chronic stress face a 20 percent higher risk of neurodegeneration, highlighting the link between lifestyle management and the degeneration process.
Avoiding Environmental Toxins and Harmful Habits
Reducing exposure to toxins and unhealthy habits is essential for slowing the degeneration process. Smoking, excessive alcohol use, and pollution all contribute to cellular damage and disease risk.
Protective measures:
- Quitting smoking and limiting alcohol intake.
- Using blue light filters on digital devices to protect vision.
- Installing air purifiers to reduce indoor pollutants.
For example, research shows that quitting smoking can halve the risk of age-related macular degeneration, underlining the impact of lifestyle choices on the degeneration process.
Regular Health Monitoring and Preventive Care
Staying on top of your health with regular monitoring is key to managing the degeneration process. Annual check-ups and screenings help catch early warning signs before they progress.
Best practices:
- Schedule annual physicals and targeted screenings for vision, cognition, and blood pressure.
- Stay up to date on vaccinations to prevent infections that can worsen chronic conditions.
- Manage existing diseases like diabetes or hypertension to reduce additional degeneration risk.
Early intervention and preventive care are powerful tools in slowing the degeneration process and maintaining independence.
Community and Social Engagement
Maintaining strong social connections supports both cognitive health and emotional well-being throughout the degeneration process. Engaging in group activities, volunteering, or playing brain games can offer protective benefits.
Consider these options:
- Join local clubs or volunteer groups to stay mentally active.
- Participate in group exercise for both physical and social benefits.
- Challenge your mind with puzzles and memory games.
Research shows that social engagement can lower dementia risk by 25 percent, emphasizing the importance of connection in the degeneration process. For more practical tips and insights, explore Uncategorized Degeneration Topics to broaden your understanding and prevention strategies.
Latest Advances and Treatment Innovations in Degeneration (2025)
Breakthroughs in the degeneration process are transforming disease management and patient outcomes in 2025. Innovations span pharmaceuticals, regenerative medicine, integrative therapies, and targeted interventions for vision loss. Understanding these advances empowers patients and clinicians to make informed choices and stay ahead of emerging treatments.
Pharmaceutical and Medical Therapies
The pharmaceutical landscape for the degeneration process is rapidly evolving. Disease-modifying drugs, such as monoclonal antibodies, are providing new hope for conditions like Alzheimer's and retinal degeneration. Stem cell therapies are also advancing, notably with Bayer advances Parkinson’s cell therapy now in Phase III trials, targeting neural restoration for Parkinson’s disease.
Recent FDA approvals highlight medications that slow progression and improve quality of life for patients with degenerative diseases. These advances offer tailored approaches, matching therapies to specific stages and types of the degeneration process. The focus is increasingly on early intervention and maximizing function.
Regenerative Medicine and Emerging Technologies
Regenerative medicine is reshaping the landscape of the degeneration process. Stem cell transplantation and tissue engineering provide options for repairing damaged tissues and organs. CRISPR gene editing is enabling personalized interventions, aiming to correct genetic defects at the source.
Excitingly, Gene therapy shows promise for Huntington’s disease by significantly slowing disease progression in clinical trials. Retinal implants are restoring vision for patients with advanced eye degeneration. These technologies represent a shift from symptom management to true restoration, redefining the future of care.
Integrative and Complementary Therapies
Integrative therapies are playing a vital role in managing the degeneration process. Nutraceuticals, such as omega-3 fatty acids and curcumin, are being studied for their neuroprotective effects. Acupuncture, especially for osteoarthritis, has demonstrated benefits in reducing pain and improving function.
Physical therapy remains essential for maintaining mobility and slowing musculoskeletal degeneration. Microacupuncture is emerging as a supportive approach for degenerative eye conditions, often used alongside conventional treatments. These evidence-based strategies offer holistic support for patients at all stages.
MicroAcupuncture Institute: A New Hope for Degenerative Eye Conditions
The MicroAcupuncture Institute is pioneering a unique approach to the degeneration process, focusing on vision loss from degenerative eye diseases. Their specialized microacupuncture techniques aim to increase blood flow and activate retinal cells, with thousands of treatments performed globally.
Patients with macular degeneration, retinitis pigmentosa, glaucoma, and optic nerve disorders have benefited from this method. The institute’s mission is to reach 1 million treatments in the next decade, offering comprehensive online training for practitioners. Growing research and patient stories highlight microacupuncture’s potential for vision restoration and hope for those affected.
If you’re concerned about the impact of degeneration on your vision or overall health, you’re not alone. As we’ve explored, early detection and proactive steps can make a real difference—especially when it comes to eye health. Our team in Tampa specializes in microacupuncture, a treatment designed to restore blood flow and revive dormant retinal cells for those living with conditions like macular degeneration, glaucoma, or optic nerve issues. If you’d like to discuss your unique situation or explore how these advances might help you or a loved one, Schedule A Free Phone Call and let’s start your journey toward clearer vision together.
