Discover how breakthroughs in eye care are revolutionizing vision health as we approach 2026. With millions managing vision challenges, understanding the eye process is more important than ever for proactive and effective care.
This guide takes you through every stage of the eye process, from the basics of eye anatomy to the latest diagnostic tools and treatment innovations. By understanding each step, you can make informed choices for your eye health and anticipate what to expect in the coming years.
Read on for a comprehensive journey into the eye process, including emerging technologies, patient experiences, and expert insights to help you achieve optimal vision in 2026.
Understanding Eye Anatomy and Function
The eye process is a remarkable journey that starts with the structure and function of the human eye. Understanding how each part contributes to vision is essential for appreciating how the eye process works and identifying where things can go wrong. Let’s explore the anatomy, the step-by-step visual pathway, and common conditions that impact the eye process.
The Structure of the Human Eye
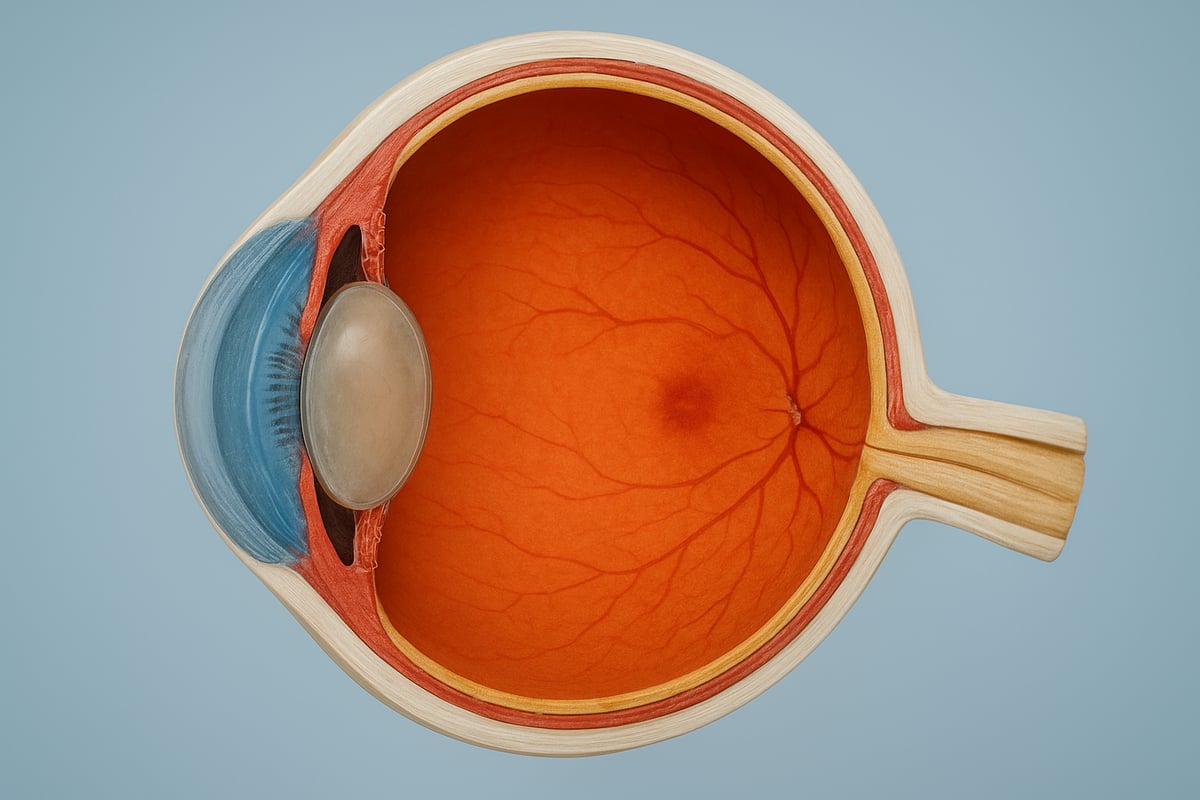
The human eye is made up of several main components, each playing a unique role in the eye process. The cornea acts as the clear front surface, bending light as it enters. Behind it, the lens fine-tunes focus, directing light toward the retina. The retina, a thin layer of tissue at the back, is responsible for converting light into neural signals.
The macula, located at the center of the retina, provides sharp central vision, while the optic nerve carries visual information to the brain. For a deeper dive into each part’s function, see Understanding the Structure of Your Eye.
For example, when light hits the retina, specialized cells instantly transform it into electrical signals, launching the eye process of vision. According to the World Health Organization, over 2.2 billion people globally have some form of vision impairment, underscoring the importance of understanding eye anatomy.
How the Eye Processes Visual Information
The eye process involves several precise steps. First, light enters through the cornea, then passes through the lens, which focuses the rays onto the retina. The retina contains photoreceptors—rods for night vision and cones for color vision—that initiate the eye process by converting light to nerve signals.
These signals travel via the optic nerve to the brain, where images are formed. For instance, cones allow us to see vibrant colors in daylight, while rods help us detect shapes in low light. The optic nerve is vital in the eye process, as it serves as the main pathway delivering information for interpretation.
Common Eye Conditions Impacting the Process
Several conditions can disrupt the normal eye process. Macular degeneration affects the macula, leading to central vision loss. Glaucoma damages the optic nerve, often resulting in peripheral vision problems. Diabetic retinopathy harms the retina due to high blood sugar, and cataracts cloud the lens, blurring vision.
Each condition alters the eye process differently. For example, age-related macular degeneration progresses by deteriorating the macula, making tasks like reading difficult. According to the CDC, macular degeneration is the leading cause of vision loss in people over 60, highlighting the need for awareness and early intervention.
The Eye Process Journey: Step-by-Step in 2026
Understanding the eye process in 2026 means following a clear pathway from prevention to rehabilitation. Each step brings new technologies and strategies to protect and restore vision. Let us walk through this journey, highlighting how innovation empowers patients at every stage.

Step 1: Preventive Eye Health and Screening
The first step in the eye process is prioritizing preventive care. In 2026, regular eye exams remain vital, but the tools have evolved. AI-based retinal scans now detect subtle changes in eye health earlier than ever. This proactive approach helps catch conditions like diabetic retinopathy before symptoms appear.
For example, a patient with diabetes may have early signs of damage identified during a routine AI-powered screening. This allows for immediate intervention and a personalized care plan. According to Prevent Blindness, 75 percent of vision loss is preventable with early intervention. Embracing preventive steps in the eye process is key to long-term vision health.
Step 2: Diagnosis and Mapping
After screening, precise diagnosis and mapping are essential in the eye process. Advanced tools such as optical coherence tomography (OCT), fundus photography, and even genetic testing provide detailed images and data. These technologies allow specialists to map the unique structure and function of each patient’s eyes.
For instance, 3D imaging of the optic nerve can reveal early signs of glaucoma or other diseases. This detailed mapping leads to more accurate diagnoses and tailored treatments. Timely and accurate diagnosis in the eye process means better outcomes and a higher chance of preserving vision.
Step 3: Treatment Pathways and Innovations
Treatment in the eye process has seen remarkable breakthroughs by 2026. Options now include pharmaceuticals, laser therapies, and minimally invasive surgeries. Even more promising are gene and stem cell therapies, some of which have received FDA approval for inherited retinal diseases.
For example, patients with genetic eye conditions may benefit from these targeted therapies, which can restore or preserve vision. Personalized medicine ensures that treatments are matched to each person’s needs. To learn more about these advancements, see Effective Treatments for Eye Conditions. Innovation at this stage of the eye process gives hope to patients with even the most complex diagnoses.
Step 4: Rehabilitation and Vision Restoration
The final step in the eye process focuses on rehabilitation and restoring quality of life. Vision therapy, assistive devices, and digital aids help patients adapt to changes in sight. Occupational therapists play a crucial role in teaching strategies for daily living and independence.
An inspiring example is the use of AR glasses, which can enhance remaining vision for those with low vision. According to the American Academy of Ophthalmology, 90 percent of low vision patients benefit from rehabilitation. Completing the eye process with strong support ensures that patients thrive, regardless of their diagnosis.
Innovations Shaping the Eye Process in 2026
Breakthroughs in technology are reshaping the eye process, offering hope to millions worldwide. Let us explore how these innovations are making vision care more effective and accessible in 2026.

Artificial Intelligence and Machine Learning
Artificial intelligence now plays a critical role in the eye process, transforming how diseases are detected and managed. AI-driven algorithms analyze retinal images, enabling faster and more accurate diagnoses. For instance, platforms like Google’s DeepMind are being used to screen for diabetic retinopathy with over 90 percent accuracy.
AI not only reduces diagnostic errors but also cuts down wait times, ensuring patients receive timely care. Deep learning models are increasingly used for eye disease classification using deep learning techniques, supporting clinicians throughout the eye process. This results in earlier intervention and better patient outcomes.
Gene and Cell Therapies
Gene and cell therapies are revolutionizing the treatment landscape within the eye process. Techniques such as CRISPR gene editing and stem cell injections now offer new hope for those with inherited retinal diseases. Luxturna, a gene therapy, has restored vision for over 1,000 patients since 2022.
These therapies target the root causes of vision loss, potentially curing conditions once deemed untreatable. The eye process now includes personalized genetic testing to identify candidates for these breakthroughs. Such advances signal a future where prevention and restoration are increasingly possible.
Smart Implants and Bionic Eyes
Smart implants and bionic eye systems add a new dimension to the eye process, especially for individuals with severe vision loss. Devices like the Argus II bionic eye help restore partial vision by converting images into electrical signals sent directly to the retina.
Recent innovations integrate these implants with neural networks, enhancing visual perception and adaptability. This technology enables those affected by blindness to regain independence and improve their quality of life. The eye process continues to evolve as these devices become more sophisticated and accessible.
Digital Health and Teleophthalmology
Digital health solutions are expanding access to eye care, making the eye process more inclusive than ever. Teleophthalmology allows patients in rural or underserved areas to receive expert consultation through smartphone apps and remote monitoring devices.
Since 2020, teleophthalmology adoption has increased by 60 percent, bridging gaps in care delivery. Digital platforms streamline appointments, follow-ups, and data sharing, empowering patients to manage their eye process from home. This innovation ensures that quality vision care reaches more people, regardless of location.
The Patient Journey: From Symptoms to Sight
Understanding the eye process from the patient's perspective is vital for timely intervention and better outcomes. Each journey is unique, but most follow a clear path from the first symptoms to potential vision restoration.

Recognizing Early Symptoms and Seeking Help
The eye process often begins with subtle warning signs. Patients may notice blurred vision, new floaters, flashes of light, or sudden vision loss. These symptoms can indicate serious conditions, including retinal detachment or acute glaucoma.
Prompt action is critical. Delaying a visit can lead to irreversible damage. For example, a patient experiencing sudden vision loss due to retinal detachment who seeks care quickly often retains more vision than someone who waits. Unfortunately, about 50 percent of patients postpone seeking help, which worsens outcomes according to the NEI.
Early recognition and response are the first steps in the eye process, and understanding their importance can prevent long-term visual impairment. For more on how vision loss statistics highlight this global challenge, see Visual impairment statistics.
Navigating the Healthcare System
Once symptoms are recognized, the next phase in the eye process involves navigating the healthcare system. Patients typically begin with a primary care provider or optometrist, who may refer them to an ophthalmologist for further evaluation.
This journey can include multiple specialist visits, diagnostic tests, and discussions about insurance coverage. Coordinated care is especially important for those with chronic conditions like diabetes, where communication between providers ensures comprehensive management.
A multidisciplinary approach in the eye process streamlines diagnosis and treatment, reducing delays and confusion. This support network helps patients make informed decisions at every stage.
Managing Treatment and Recovery
Managing the treatment phase of the eye process requires education and active participation. Patients must understand their options, from eye drops and medications to surgeries or new therapies.
Adherence is essential. For example, glaucoma patients who consistently use prescribed eye drops have a significantly lower risk of vision loss compared to those who skip doses. Non-adherence increases this risk by 30 percent, as reported by the Glaucoma Research Foundation.
For those with degenerative conditions, learning about the Degeneration Process in Eyes can help clarify why recovery may be complex. Staying informed empowers patients to work closely with their care team for the best possible outcomes in the eye process.
Emotional and Social Support
The emotional impact of vision changes can be profound. Patients navigating the eye process may experience anxiety, frustration, or depression as they adapt to new realities.
Support is available. Counseling, peer support groups, and rehabilitation services can make a significant difference. For instance, those with macular degeneration often benefit from connecting with others facing similar challenges.
Holistic care in the eye process addresses not only the medical aspects but also the emotional and social needs, ensuring patients are supported throughout their journey.
Future Trends in Eye Process and Vision Care
The future of vision care is rapidly evolving, with the eye process at the center of technological advancements and patient-centered solutions. As we look toward 2026, groundbreaking innovations are making personalized, accessible, and effective eye health a reality for more people than ever before.
Predictive Analytics and Personalized Medicine
Predictive analytics is transforming the eye process by harnessing big data to anticipate and prevent vision problems before they escalate. Advanced algorithms analyze patient histories, genetic data, and lifestyle factors to identify those at risk for specific eye diseases.
For example, clinicians can now use risk stratification models to tailor screening schedules for glaucoma patients. This shift means each step of the eye process is uniquely adapted to the individual, improving early intervention rates and outcomes.
The result is a move from reactive care to proactive, data-driven strategies that empower both patients and providers.
Integration of Wearable Technology
Wearable technology is reshaping the eye process by enabling real-time monitoring and early detection. Smart contact lenses and wearable sensors now track intraocular pressure, glucose levels, and other vital metrics continuously.
A notable example is glucose-sensing contact lenses for diabetics, which alert users to changes that could impact their vision. According to MarketWatch, the wearables market for eye care is projected to reach $2 billion by 2026.
These innovations make the eye process more dynamic, offering patients a hands-on role in managing their own vision health.
Accessibility and Global Vision Initiatives
Expanding access to quality eye care is a major goal for the future. Global initiatives like WHO’s Vision 2030 aim to bridge gaps in the eye process for underserved communities. Mobile clinics, telemedicine, and public health campaigns are making screenings and treatments available in remote areas.
Despite progress, 1 billion people worldwide still lack basic eye care. Disparities are also evident in the prevalence of diseases like glaucoma, which you can learn more about in the Global prevalence of glaucoma overview.
By focusing on outreach and innovative delivery models, the eye process is becoming more equitable and far-reaching.
Ongoing Research and Clinical Trials
Research into the eye process continues to unlock new possibilities for vision restoration and disease management. Areas such as retinal regeneration, neuroprotection, and nanomedicine are at the forefront of clinical trials.
For example, new neuroprotective drugs are being tested for glaucoma, offering hope for slowing or halting disease progression. Patients interested in participating in research will find more opportunities as studies expand.
The future of the eye process promises ongoing advancements, making sight preservation more achievable for all.
As you’ve discovered throughout this guide, understanding the eye process and staying informed about the latest breakthroughs can make a real difference in your vision health—especially if you or someone you love faces conditions like macular degeneration or glaucoma. If you’re curious about how innovative treatments like MicroAcupuncture could help restore your sight or simply want clear, expert guidance on your next steps, I invite you to take the first step toward better vision.
Schedule A Free Phone Call
and let’s explore your options together.
